Non-invasive ventilation (NIV) is the delivery of ventilatory support without the need for an invasive artificial airway. Mechanical ventilation via intubation is associated with many complications, including upper airway trauma, arrhythmia, hypotension, aspiration of gastric contents, sinusitis, pneumonia, and patients' loss of ability to eat and communicate verbally.
The concept of mechanical ventilation first evolved with negative-pressure ventilation when the "iron lung" was
initially developed in the early 1900s and was used extensively during the polio epidemics of the 1940s and
1950s. The iron lung works by augmenting the tidal volume by applying negative extrathoracic pressure. These ventilators fell out of favor as the use of invasive positive-pressure ventilation (PPV) increased during the 1960s. Fueled by the development of PPV delivered through a nasal or face mask, a dramatic resurgence has occurred in the use of NIV over the past decade. NIV
currently has a definite and emerging role in the management of acute and chronic respiratory failure of
many etiologies.1,2
Non-Invasive PPV
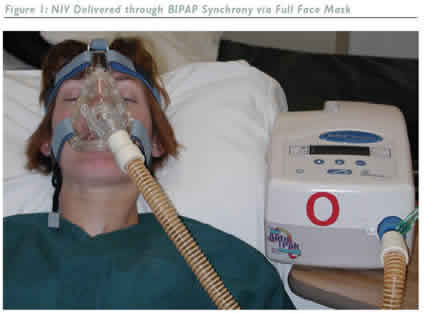
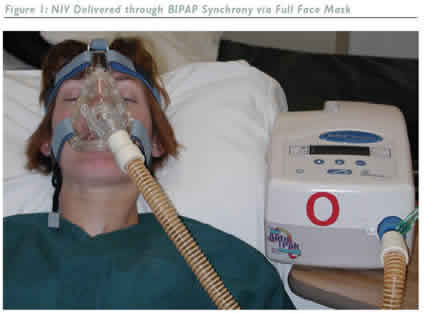
Non-invasive PPV (NPPV) is delivered through a nasal or face mask, eliminating the need for intubation or tracheostomy. NPPV can be given through a volume ventilator, a pressure-controlled ventilator, a bi-level positive airway pressure (BIPAP or bi-level ventilator) device, or a continuous positive airway pressure (CPAP) device. BIPAP, the most commonly used modality, provides continuous high-flow positive airway pressure that cycles between a high inspiratory positive airway
pressure (IPAP) and a lower expiratory positive airway pressure (EPAP).1,2 Although positive pressure support is
usually well tolerated by patients, mouth leaks or other difficulties are sometimes encountered. NIV may be
used as a continuous or intermittent mode of assistance depending on the patient's clinical situation. Instantaneous and steady support is given to patients in acute respiratory distress. As the underlying condition improves, ventilator-free periods are increased as tolerated, and support is discontinued when the patient is deemed stable. The total duration of ventilator use
varies with the underlying disease-approximately six hours for acute pulmonary edema, but more than two days for chronic obstructive pulmonary disease (COPD) exacerbation.
Mechanisms of Action
NPPV decreases the work of breathing and thereby improves alveolar ventilation while simultaneously resting the respiratory musculature. The improvement in gas exchange with BIPAP occurs because of an increase in alveolar ventilation. Externally applied EPAP decreases the work of breathing by partially overcoming the auto-positive end-expiratory pressure (PEEP) as patients generate less negative inspiratory force to initiate the breathing cycle. In spontaneous mode, higher pressure is delivered upon detection of
inspiration until the flow rate falls below the threshold level. The expiratory pressure with bi-level pressure support is equivalent to the PEEP, and the inspiratory pressure is equivalent to the sum of the PEEP and the level of pressure support. In timed mode, bi-phasic positive airway pressure ventilation alternates between the inspiratory and expiratory pressures at fixed time intervals, which allows unrestricted breathing at both pressures. Supplemental oxygen can be connected to the device, but a higher flow of oxygen therapy is then usually required.
Effectiveness of NIV should be determined clinically through amelioration of respiratory distress, patient discomfort and improved results from arterial blood gas determinations.The decision to use a nasal mask or a full face mask depends on the patient's preference and tolerance.
Patient Selection
Patients who are in acute respiratory distress and are at risk of needing intubation should be selected for NIV if they have a reversible cause of acute respiratory failure.3,4 Most patients requiring NPPV should be managed in the intensive care unit (ICU) setting. Once stabilized, weaning from NPPV may be accomplished either by progressively decreasing the levels of positive airway pressure or by withholding NIV for increasing lengths of time. A combination of both strategies can also be used. Indications, contraindications, and factors predicting success are listed in Tables 1, 2, and 3.
NIV in Acute Exacerbation of COPD
Patients with acute exacerbation of COPD (AECOPD) develop deterioration of gas exchange accompanied by rapid shallow breathing, severe dyspnea, right ventricular failure, and encephalopathy. Respiratory mechanical abnormalities lead to inadequate alveolar ventilation, shortened inspiratory time, diminished tidal volume, and increased respiratory frequency. NIV increases alveolar
ventilation and reduces the loads imposed on the respiratory muscles. In acute respiratory failure in
patients with COPD, NPPV offers a number of potential advantages over invasive PPV.5,6 These advantages include avoidance of intubation-related trauma, a decreased incidence of nosocomial pneumonia, enhanced patient comfort, a shorter duration of ventilator use, a reduction in hospital stay, and, ultimately, reduced healthcare costs.
In a randomized trial comparing NPPV with a standard ICU approach, the use of NPPV was shown to reduce complications, duration of ICU stay, and mortality.7 Plant et al. recently published another large prospective randomized study comparing NPPV with the standard treatment in patients with COPD exacerbation.8 Treatment failed in significantly more patients on
conventional therapy compared with the control group (27% versus 15%). In-hospital mortality rates were
significantly reduced in patients treated with NPPV (from 20% to 10%). Additionally, other prospective and
cohort studies with historical or matched control groups have suggested that long-term outcome with
NPPV is much better compared with medical therapy and/or endotracheal intubation.9-13
NIV in Hypoxemic Respiratory Failure
Studies on the use of NPPV in hypoxemic respiratory failure have yielded conflicting results. This category
comprises patients with a variety of diagnoses, e.g. pneumonia, congestive heart failure, and acute respiratory distress syndrome.14-16 Uncontrolled studies have suggested that some patients with hypoxemic respiratory failure may respond favorably to NPPV. In one study of 64 patients with hypoxemic respiratory failure, NPPV reduced the duration of mechanical
ventilation (three versus six days), the length of ICU stay (three versus six days), and serious complications.17 Another study compared BIPAP with high-flow oxygen therapy in patients with acute hypoxemic respiratory failure. NPPV was associated with decreased need for intubation (25% versus 52%), improved ICU mortality (18% versus 39%) and increased 90-day survival.18 Although these results appear to be encouraging, the use of NPPV in patients with hypoxemic respiratory failure requires further investigation before its widespread clinical use.
NIV in Other Causes of Acute Respiratory Failure
Although controlled studies are lacking, several case series report successful NPPV use in acute asthma, cystic fibrosis, respiratory deterioration following extubation, and as a method of weaning patients from invasive ventilation.19-21 The exception is acute pulmonary edema, where CPAP has been shown to be an effective therapy for improving gas exchange,
decreasing respiratory work, and reducing the rate of endotracheal intubation.22 In a controlled study, nasal BIPAP improved the partial pressure of carbon dioxide in arterial gas (PaCO2) levels, pH, respiratory rate, and dyspnea more rapidly than nasal CPAP in patients with acute pulmonary edema.23 CPAP may appear to be a logical first choice in the treatment of these patients; however, patients with hypercapnia or continued respiratory distress on CPAP should be switched to
BIPAP.24,25 Patients with acute or chronic respiratory failure secondary to obesity hypoventilation syndrome
may be treated with NPPV or, if intubated, may be weaned from invasive ventilation to NPPV support.26,27
These patients require ventilatory support, initially 24 hours a day and, subsequently, night-time weaning via
NPPV appears to be an excellent option.
NIV in Chronic Restrictive Thoracic Disorders
Nocturnal NIV is an effective treatment for hypercapnic respiratory failure in patients with restrictive thoracic
disease. Respiratory failure is reversed by increasing the ventilatory response to CO2, reducing inspiratory muscle fatigue, or enhancing pulmonary mechanics. Several uncontrolled and controlled studies have demonstrated that even patients with severe CO2 retention and symptoms such as morning headache and daytime hypersomnolence could undergo remarkable reversal after several weeks of nocturnal NIV.28-30 Longterm survival of patients on NPPV who develop chronic respiratory failure because of restrictive thoracic diseases is comparable with survival of those patients who use invasive PPV. However, NPPV is associated with fewer
deaths. NPPV should be initiated at the onset of daytime hypoventilation and symptoms as early institution may be advantageous in slowing the progression of respiratory failure. At later stages, invasive PPV may need to be instituted, although on-going use of NPPV has been advocated.
Complications of NPPV
The most common nuisance with NPPV is local damage to the facial tissue from pressure effects of the mask and straps. Mild gastric distension may occur, but is not significant; removal of the nasogastric tube is not warranted. Eye irritation and sinus pain or congestion may also occur. Barotrauma is uncommon, but adverse hemodynamic effects from NIV may occur. Modest air
leaks at the facial seal are common, but are tolerated and of no consequence. Patients on NPPV must be
carefully monitored for patient comfort, worsening respiratory distress, and hypoxemia. For a variety of
reasons, NIV is not always successful. Indicators of failure, such as hemodynamic instability, deteriorating
mental status, and an increasing respiratory rate should be closely monitored.
Conclusion
More clinical research is needed before NPPV can be used to its greatest advantage in respiratory failure from
a wide variety of causes. Advances in interface and ventilator technology will likely enhance patient
tolerance. The recent increase in NPPV use in acute case settings has been encouraged by the desire to
reduce the complications arising from intubation and invasive ventilation.Although NIV has well-established
efficacy in AECOPD, acute pulmonary edema, and restrictive neuromuscular disorders, further research is
needed to define its role in hypoxemic respiratory failure and other causes of acute and chronic
respiratory failure.
References
- Sharma S,"Non invasive Ventilation", http://www.emedicine.com/med/topic3371.htm (accessed on November 30 2005).
- Mehta S, Hill N S, "Noninvasive Ventilation: State of the art", Am. J. Respir. Crit. Care Med. (2001);163: pp. 540-577.
- Brochard, Mancebo J, Elliot M W,"Noninvasive ventilation for acute respiratory failure", Eur. Respir. J. (2002);19(4): pp. 712-721.
- Phua J, Kong K, Lee K H et al., "Noninvasive ventilation in hypercapnic acute respiratory failure due to chronic obstructive
pulmonary disease vs. other conditions: effectiveness and predictors of failure", Intensive Care Med. (2005);31(4): pp. 533-539.
- Ambrosino N, Foglio K, Rubini F et al.,"Non-invasive mechanical ventilation in acute respiratory failure due to chronic obstructive
pulmonary disease: correlates for success", Thorax (1995);50(7): pp. 755-757.
- Keenan S P, Kernerman P D, Cook D J et al.,"Effect of noninvasive positive pressure ventilation on mortality in patients admitted
with acute respiratory failure: a meta-analysis", Crit. Care Med. (1997);25: pp. 1,685-1,692.
- Brochard L, Mancebo J,Wysocki M et al., "Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary
disease", N. Engl. J. Med. (1995);333: pp. 817-822.
- Plant P K, Owen J L, Elliot M W,"Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary
disease on general respiratory wards: a multicentre randomised controlled trial", Lancet (2000);355: pp. 1,931-1,935.
- Appendini L, Patessio A, Zanaboni S et al."Physiologic effects of positive end-expiratory pressure and mask pressure support during exacerbations of chronic obstructive pulmonary disease", Am. J. Respir. Crit. Care Med. (1994);149(5): pp. 1,069-1,076.
- Bott J, Carroll M P, Conway J H et al.,"Randomised controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease", Lancet (1993);341(8,860): pp. 1,555-1,557.
- Bersten A D, Holt A W,Vedig A E et al., "Treatment of severe cardiogenic pulmonary edema with continuous positive airway pressure delivered by face mask", N. Engl. J. Med. (1991);325(26): pp. 1,825-1,830.
- Brochard L, Isabey D, Piquet J et al.,"Reversal of acute exacerbations of chronic obstructive lung disease by inspiratory assistance with a face mask", N. Engl. J. Med. (1990);323(22): pp. 1,523-1,530.
- Celikel T, Sungur M, Ceyhan B et al., "Comparison of noninvasive positive pressure ventilation with standard medical therapy
in hypercapnic acute respiratory failure", Chest (1998);114(6): pp. 1,636-1,642.
- Ferrer M, Esquinas A, Leon M et al., "Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical
trial", Am. J. Respir. Crit. Care Med. (2003);168(12): pp. 1,438-1,444.
- Delclaux C, L'Her E,Alberti C, Mancebo J,Abroug F, Conti G et al.,"Treatment of acute hypoxemic nonhypercapnic respiratory
insufficiency with continuous positive airway pressure delivered by a face mask: A randomized controlled trial", JAMA
(2000);284(18): pp. 2,352-2,360.
- Hilbert G, Gruson D,Vargas F et al., "Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure", N. Engl. J. Med. (2001);344(7): pp. 481-487.
- Antonelli M, Conti G, Rocco M et al., "A comparison of noninvasive positive-pressure ventilation and conventional mechanical ventilation in patients with acute respiratory failure", N. Engl. J. Med. (1998);339: pp. 429-435.
- Wood K A, Lewis L,Von Harz B et al.,"The use of noninvasive positive pressure ventilation in the emergency department: results of a randomized clinical trial", Chest (1998);113: pp. 1,339-1,346.
- Meduri G U, Cook T R, Turner R E et al., "Noninvasive positive pressure ventilation in status asthmaticus", Chest (1996);110(3): pp. 767-774.
- Granton J T, Kesten S, "The acute effects of nasal positive pressure ventilation in patients with advanced cystic fibrosis", Chest (1998);113(4): pp. 1,013-1,018.
- Ferrer M, Esquinas A, Arancibia F et al., "Noninvasive ventilation during persistent weaning failure: a randomized controlled trial", Am. J. Respir. Crit. Care Med. (2003);168(1): pp. 70-76.
- Nava S, Carbone G, DiBattista N et al., "Noninvasive ventilation in cardiogenic pulmonary edema: a multicenter randomized trial", Am. J. Respir. Crit. Care Med. (2003);168(12): pp. 1,432-1,437.
- Mehta S, Jay G D,Woolard R H et al., "Randomized, prospective trial of bilevel versus continuous positive airway pressure in acute pulmonary edema", Crit. Care Med. (1997);25(4): pp. 620-628.
- Crane S D, Elliot M W, Gilligan P et al., "Randomised controlled comparison continuous positive airways pressure, bilevel noninvasive ventilation, and standard treatment in emergency department patients with acute cardiogenic pulmonary edema", Emerg. Med. J. (2004);21: pp. 155-161.
- Mossip J, Paez J, Merino M et al.,"Risk factors for intubation as a guide for noninvasive ventilation in patients with severe acute
cardiogenic pulmonary edema", Intensive Care Med. (2003);29: pp. 1,921-1,928.
- Masa J F, Celli B R, Riesco J A et al., "The obesity hypoventilation syndrome can be treated with noninvasive mechanical
ventilation", Chest (2001);119(4): pp. 1,102-1,107.
- Perez de Llano L A, Golpe R, Ortiz Piquer M et al., "Short-term and long-term effects of nasal intermittent positive pressure ventilation in patients with obesity-hypoventilation syndrome", Chest (2005);128(2): pp. 587-594.
- Nickol A H, Hart N, Hopkinson N S et al.,"Mechanisms of improvement of respiratory failure in patients with restrictive thoracic
disease treated with non-invasive ventilation", Thorax (2005);60(9): pp. 754-760.
- Ergun P,Aydin G,Turay UY et al.,"Short-term effect of nasal intermittent positive-pressure ventilation in patients with restrictive
thoracic disease", Respiration (2002);69(4): pp. 303-308.
- Leger P, Jennequin J, Gerard M et al., "Home positive pressure ventilation via nasal mask for patients with neuromusculoskeletal
disorders", Eur. Respir. J. Suppl. (1989);7: pp. 640s-644s.
Sat Sharma, MD, FRCPC, FCCP, FACP,is Associate Professor in the Sections of Respirology and Critical
Care of the Department of Internal Medicine at the University of Manitoba, Winnipeg, Canada. He is also Program Director of postgraduate education in respirology at the same university and Site Director of respiratory medicine at St Boniface General Hospital. Professor Sharma's other national and international appointments include Chair of the Specialty Committee in Respirology of the Royal College of Physicians and Surgeons of Canada (RCPSC), Governor of the Manitoba chapter of the American College of Chest
Physicians (ACCP), member of the Health and Science Policy Committee of the ACCP, and member of the Canadian Thoracic
Society Board. Professor Sharma's research interests involve studying the epidemiology of respiratory
diseases, perioperative respiratory care, exercise-induced hypoxemia, and therapeutic clinical research.
©Copyright All Rights Reserved
DO NOT REPRODUCE WITHOUT WRITTEN PERMISSION BY AUTHOR.